4-Hydroxyamphetamine
 | |
| Clinical data | |
|---|---|
| Trade names | Paredrine, Paremyd, Pedrolon, Mycadrine, Paredrinex, others |
| Other names | 4-Hydroxyamphetamine; 4-HA; Hydroxyamfetamine; Oxamphetamine; Norpholedrine; para-Hydroxyamphetamine; PHA; α-Methyltyramine; Methyltyramine, Hydroxyamphetamine (USAN US) |
| Routes of administration | Eye drops |
| ATC code |
|
| Legal status | |
| Legal status |
|
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.002.866 |
| Chemical and physical data | |
| Formula | C9H13NO |
| Molar mass | 151.209 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
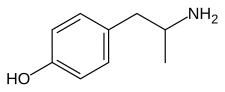
Hydroxyamphetamine, also known as 4-hydroxyamphetamine or norpholedrine and sold under the brand names Paredrine and Paremyd among others, is a sympathomimetic medication used in eye drops to dilate the pupil for eye examinations.[1][2][3][4]
Hydroxyamfetamine acts as a norepinephrine releasing agent and hence is an indirectly acting sympathomimetic.[5][6] It is a substituted phenethylamine and amphetamine.[4]
Hydroxyamphetamine appeared to remain marketed only in the Czech Republic as of 2004.[3]
Medical uses
Hydroxyamphetamine is used in eye drops to dilate the pupil (a process called mydriasis) so that the back of the eye can be examined. This is a diagnostic test for Horner's syndrome. Patients with Horner's syndrome exhibit anisocoria brought about by lesions on the nerves that connect to the nasociliary branch of the ophthalmic nerve.[7] Application of hydroxyamphetamine to the eye can indicate whether the lesion is preganglionic or postganglionic based on the pupil's response. If the pupil dilates, the lesion is preganglionic. If the pupil does not dilate, the lesion is postganglionic.[7]
Hydroxyamphetamine has some limitations to its use as a diagnostic tool. If it is intended as an immediate follow up to another mydriatic drug (cocaine or apraclonidine), then the patient must wait anywhere from a day to a week before hydroxyamphetamine can be administered.[8][5] It also has the tendency to falsely localize lesions. False localization can arise in cases of acute onset; in cases where a postganglionic lesion is present, but the nerve still responds to residual norepinephrine; or in cases in which unrelated nerve damage masks the presence of a preganglionic lesion.[7][8]
Available forms
Hydroxyamphetamine is a component of two controlled (prescription only), name-brand ophthalmic mydriatics: Paredrine and Paremyd. Paredrine consists of a 1% solution of hydroxyamphetamine hydrobromide[9]: 543 while Paremyd consists of a combination of 1% hydroxyamphetamine hydrobromide and 0.25% tropicamide.[10]
Pharmacology
Pharmacodynamics
Hydroxyamphetamine acts as an indirect sympathomimetic and induces the release of norepinephrine which leads to mydriasis (pupil dilation).[5][6]
It has also been found to act as a serotonin releasing agent.[11] The drug produces the head-twitch response, a behavioral proxy of psychedelic effects, when it is given by intracerebroventricular injection in animals.[11] This effect is blocked by the serotonin receptor antagonists cyproheptadine and dimethothiazine, by the serotonin reuptake inhibitor fluoxetine, and by the serotonin synthesis inhibitor para-chlorophenylalanine (PCPA).[11] These findings suggest that hydroxyamphetamine-induced head twitches are due to activation of the serotonin 5-HT2A receptor and that they are mediated by induction of serotonin release as opposed to direct agonism of the serotonin 5-HT2A receptor.[11] Although hydroxyamphetamine produces the head-twitch response in animals, serotonin releasing agents are not necessarily hallucinogenic in humans, and hence their induction of head twitches in animals has been considered a false positive for psychedelic effects.[12][13][14]
It additionally decreases metabolism of serotonin and certain other monoamines by inhibiting the activity of monoamine oxidases (MAOs), particularly type A (MAO-A). The inhibition of MAO-A prevents metabolism of serotonin and catecholamines in the presynaptic terminal, and thus increases the amount of neurotransmitters available for release into the synaptic cleft.[11]
Like amphetamine, hydroxyamphetamine is an agonist of human TAAR1.[15]
Pharmacokinetics
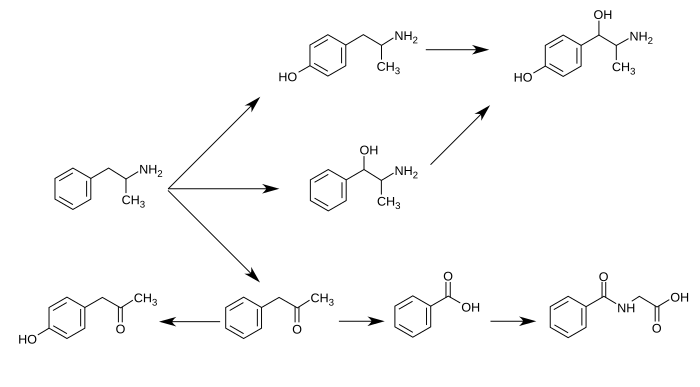
Hydroxyamphetamine is a major metabolite of amphetamine and a minor metabolite of methamphetamine. In humans, amphetamine is metabolized to hydroxyamphetamine by CYP2D6, which is a member of the cytochrome P450 superfamily and is found in the liver.[16][17] 4-Hydroxyamphetamine is then metabolized by dopamine β-hydroxylase into 4-hydroxynorephedrine or eliminated in the urine.[6]
Metabolic pathways of amphetamine in humans[sources 1]
|
Chemistry
Hydroxyamphetamine, also known as 4-hydroxy-α-methylphenethylamine, 4-hydroxyamphetamine, or α-methyltyramine, is a substituted phenethylamine and amphetamine derivative. It is the 4-hydroxylated analogue of amphetamine, the N-demethylated analogue of pholedrine (4-hydroxy-N-methylamphetamine), and the α-methylated analogue of tyramine (4-hydroxyphenethylamine). Other analogues include α-methyldopamine, corbadrine (levonordefrin; α-methylnorepinephrine), and dioxifedrine (α-methylepinephrine).
It has a predicted log P of 0.58 to 1.4.[18][4][19]
Hydroxyamphetamine is used pharmaceutically as the hydrobromide salt.[1]
History
Hydroxyamphetamine was first synthesized by 1910.[1]
In the 1990s, the trade name rights, patents, and new drug applications (NDAs) for Paredrine and Paremyd were exchanged among a few different manufacturers after a shortage of the raw material required for their production, which caused both drugs to be indefinitely removed from the market.[20] Around 1997, Akorn, Inc., obtained the rights to both Paredrine and Paremyd,[21] and in 2002, the company reintroduced Paremyd to the market as a fast acting ophthalmic mydriatic agent.[10][22][23]
In 2004, hydroxyamphetamine appeared to remain marketed only in the Czech Republic.[3]
Society and culture
Names
Hydroxyamphetamine is the generic name of the drug and its BAN and DCF, while hydroxyamfetamine is its INN.[1][2][3] In the case of the hydrobromide salt, its generic name is hydroxyamphetamine hydrobromide and this is its USAN.[1][2][3] It is also known by synonyms including methyltyramine, norpholedrine, and oxamphetamine.[1][2][3][18] The drug is sold under brand names including Paredrine, Paredrinex, Paremyd, Pedrolon, and Mycadrine.[1][3]
Other drugs
4-Hydroxyamphetamine is also a metabolite of amphetamine and certain other amphetamines.[2]
Notes
- ↑ 4-Hydroxyamphetamine has been shown to be metabolized into 4-hydroxynorephedrine by dopamine beta-hydroxylase (DBH) in vitro and it is presumed to be metabolized similarly in vivo.'"`UNIQ--ref-0000004F-QINU`"''"`UNIQ--ref-00000050-QINU`"' Evidence from studies that measured the effect of serum DBH concentrations on 4-hydroxyamphetamine metabolism in humans suggests that a different enzyme may mediate the conversion of 4-hydroxyamphetamine to 4-hydroxynorephedrine;'"`UNIQ--ref-00000051-QINU`"''"`UNIQ--ref-00000052-QINU`"' however, other evidence from animal studies suggests that this reaction is catalyzed by DBH in synaptic vesicles within noradrenergic neurons in the brain.'"`UNIQ--ref-00000053-QINU`"''"`UNIQ--ref-00000054-QINU`"'
Reference notes
- ↑ '"`UNIQ--ref-00000046-QINU`"''"`UNIQ--ref-00000047-QINU`"''"`UNIQ--ref-00000048-QINU`"''"`UNIQ--ref-00000049-QINU`"''"`UNIQ--ref-0000004A-QINU`"''"`UNIQ--ref-0000004B-QINU`"''"`UNIQ--ref-0000004C-QINU`"''"`UNIQ--ref-0000004D-QINU`"'
References
- 1 2 3 4 5 6 7 Elks J (2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer US. p. 74. ISBN 978-1-4757-2085-3. Retrieved August 30, 2024.
- 1 2 3 4 5 Morton IK, Hall JM (2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Netherlands. p. 90. ISBN 978-94-011-4439-1. Retrieved August 30, 2024.
- 1 2 3 4 5 6 7 Schweizerischer Apotheker-Verein (2004). Index Nominum: International Drug Directory. Medpharm Scientific Publishers. p. 609. ISBN 978-3-88763-101-7. Retrieved August 30, 2024.
- 1 2 3 "Hydroxyamphetamine: Uses, Interactions, Mechanism of Action". DrugBank Online. January 30, 1992. Retrieved August 30, 2024.
- 1 2 3 Lepore FE (1985). "Diagnostic pharmacology of the pupil". Clinical Neuropharmacology. 8 (1): 27–37. doi:10.1097/00002826-198503000-00003. PMID 3884149.
- 1 2 3 Cho AK, Wright J (February 1978). "Pathways of metabolism of amphetamine and related compounds". Life Sciences. 22 (5): 363–372. doi:10.1016/0024-3205(78)90282-5. PMID 347211.
- 1 2 3 Walton KA, Buono LM (December 2003). "Horner syndrome". Current Opinion in Ophthalmology. 14 (6): 357–363. doi:10.1097/00055735-200312000-00007. PMID 14615640. S2CID 11262166.
- 1 2 Davagnanam I, Fraser CL, Miszkiel K, Daniel CS, Plant GT (March 2013). "Adult Horner's syndrome: a combined clinical, pharmacological, and imaging algorithm". Eye. 27 (3): 291–298. doi:10.1038/eye.2012.281. PMC 3597883. PMID 23370415.
- ↑ Slamovits TL, Glaser JS (1999). "The Pupils and Accommodation.". In Glaser JS (ed.). Neuro-ophthalmology. Philadelphia, PA: Lippincott, Williams, & Wilkins. ISBN 978-0781717298.
- 1 2 "Hydroxyamphetamine Hydrobromide; Tropicamide". Orange Book: Approved Drug Products with Therapeutic Equivalence Evaluations. Archived from the original on March 4, 2016.
- 1 2 3 4 5 Nakagawasai O, Arai Y, Satoh SE, Satoh N, Neda M, Hozumi M, et al. (January 2004). "Monoamine oxidase and head-twitch response in mice. Mechanisms of alpha-methylated substrate derivatives". Neurotoxicology. 25 (1–2): 223–232. Bibcode:2004NeuTx..25..223N. doi:10.1016/S0161-813X(03)00101-3. PMID 14697897.
- ↑ Halberstadt AL, Geyer MA (2018). "Effect of Hallucinogens on Unconditioned Behavior". In Halberstadt AL, Vollenweider FX, Nichols DE (eds.). Behavioral Neurobiology of Psychedelic Drugs. Current Topics in Behavioral Neurosciences. Vol. 36. Berlin, Heidelberg: Springer Berlin Heidelberg. pp. 159–199. doi:10.1007/7854_2016_466. ISBN 978-3-662-55878-2. PMC 5787039. PMID 28224459.
Amphetamine and methamphetamine, which act primarily by increasing carrier-mediated release of dopamine and norepinephrine, do not provoke head twitches (Corne and Pickering 1967; Silva and Calil 1975; Yamamoto and Ueki 1975; Jacobs et al. 1976; Bedard and Pycock 1977; Halberstadt and Geyer 2013). By contrast, the 5-HT releasing drugs fenfluramine and p-chloroamphetamine (PCA) do produce a robust HTR (Singleton and Marsden 1981; Darmani 1998a). Fenfluramine and PCA are thought to act indirectly, by increasing carrier-mediated release of 5-HT, because the response can be blocked by inhibition of the 5-HT transporter (Balsara et al. 1986; Darmani 1998a) or by depletion of 5-HT (Singleton and Marsden 1981; Balsara et al. 1986). [...] Because indirect 5-HT agonists such as fenfluramine, PCA, and 5-HTP are not hallucinogenic (Van Praag et al. 1971; Brauer et al. 1996; Turner et al. 2006), their effects on HTR can potentially be classified as false-positive responses.
- ↑ Halberstadt AL, Chatha M, Klein AK, Wallach J, Brandt SD (May 2020). "Correlation between the potency of hallucinogens in the mouse head-twitch response assay and their behavioral and subjective effects in other species". Neuropharmacology. 167: 107933. doi:10.1016/j.neuropharm.2019.107933. PMC 9191653. PMID 31917152.
Indirect 5-HT2A agonists such as fenfluramine, p-chloroamphetamine (PCA), and 5-hydroxytryptophan (5-HTP) induce head twitches in rodents (Corne et al. 1963; Singleton and Marsden 1981; Darmani 1998) but do not act as hallucinogens in humans (van Praag et al. 1971; Brauer et al. 1996; Turner et al. 2006), However, overdoses of compounds that increase serotonin (5-HT) release can result in 5-HT syndrome, which sometimes includes hallucinations (Birmes et al. 2003; Evans and Sebastian 2007).
- ↑ Wojtas A, Gołembiowska K (December 2023). "Molecular and Medical Aspects of Psychedelics". Int J Mol Sci. 25 (1): 241. doi:10.3390/ijms25010241. PMC 10778977. PMID 38203411.
While some false positives have been identified, such as fenfluramine, p-chloroamphetamine, and 5-hydroxytryptophan, the test predominantly exhibits specificity for 5-HT2A receptor agonists [15].
- ↑ Lewin AH, Miller GM, Gilmour B (December 2011). "Trace amine-associated receptor 1 is a stereoselective binding site for compounds in the amphetamine class". Bioorganic & Medicinal Chemistry. 19 (23): 7044–7048. doi:10.1016/j.bmc.2011.10.007. PMC 3236098. PMID 22037049.
- ↑ Markowitz JS, Patrick KS (2001). "Pharmacokinetic and pharmacodynamic drug interactions in the treatment of attention-deficit hyperactivity disorder". Clinical Pharmacokinetics. 40 (10): 753–772. doi:10.2165/00003088-200140100-00004. PMID 11707061. S2CID 20884365.
- ↑ Haefely W, Bartholini G, Pletscher A (1976). "Monoaminergic drugs: general pharmacology". Pharmacology & Therapeutics B. 2 (1): 185–218. doi:10.1016/0306-039x(76)90030-1. PMID 817330.
- 1 2 "4-(2-Aminopropyl)phenol". PubChem. Retrieved August 30, 2024.
- ↑ "C9H13NO". Hydroxyamphetamine. August 30, 2024. Retrieved August 30, 2024.
- ↑ "Akorn Acquires Paredrine - Specialty Ophthalmic Diagnostic Product From Pharmics, Inc". Akorn press release. March 24, 1999. Archived from the original on September 16, 2018. Retrieved December 9, 2014.
- ↑ "Akorn press release". Archived from the original on December 9, 2014.
- ↑ "Akorn timeline". Archived from the original on June 26, 2019. Retrieved December 9, 2014.
- ↑ Lurcott R (December 1, 2002). "Unique Mydriatic Returns: The combination formula fosters patient flow efficiencies". Ophthalmology Management.
External links
- p-Hydroxyamphetamine at the U.S. National Library of Medicine Medical Subject Headings (MeSH)